
Clinical
How to Talk to Your Patients About BHRT
By Belmar Pharma SolutionsYour bustling, successful practice is full of women who really care about their appearance, and they trust ...
Posted By Madilyn Moeller, Wednesday, November 13, 2024

By Taylor Siemens, NP-C
Patient safety is paramount in any medical setting, and medical spas are no exception. With the growing popularity of the aesthetic medicine industry, it’s crucial that practitioners maintain the highest standards of care. While most owners and practitioners understand this responsibility, many are unaware of the tangible steps they can take to ensure patient safety throughout all aspects of their business.
Patient safety is not just a regulatory requirement—it’s the foundation of patient trust and the key to a successful practice. A single incident of malpractice or negligence can damage a practice’s reputation and lead to legal consequences; more importantly, it can harm the patient physically and emotionally. Therefore, implementing robust safety protocols is essential for every medical spa. Because medical aesthetics practices are non-traditional medical settings, the importance of regulatory training and staff competency seems to be an afterthought for some.
All staff members, from front-of-house members and non-clinicians to practitioners, should undergo continuous education. If you come from a traditional medicine setting, you likely remember the countless hours spent on staying up-to-date on policy changes and understanding protocols. This shouldn’t stop in aesthetic medicine. Ensuring your team is spending time attending workshops, webinars and certification programs is vital to patient safety and the safety of the business. Keeping up with the latest techniques, products and safety protocols ensures that everyone is knowledgeable and capable.
Regular skill assessments and case reviews are critical components of ensuring patient safety and maintaining high standards of care in medical spas. These processes help identify areas for improvement, ensure compliance with best practices and foster a culture of continuous learning. Performing case reviews on client outcomes that were negative (and positive) is a great way to ensure all team members have the opportunity for dialogue and to learn from others’ experiences.
Conduct competency evaluations at least annually for every service offered by each provider. For new staff, consider more frequent assessments—quarterly, perhaps—during their initial year of employment. There are several ways evaluations can be performed. Practical exams allow for practitioners to demonstrate their skills in performing common procedures under observation. This ensures they can apply theoretical knowledge in real-life practice. Written tests can assess knowledge of protocols, contraindications, emergency procedures and the latest industry developments. Peer reviews allow for colleagues to observe and provide feedback on each other’s techniques. This promotes a collaborative learning environment and helps identify subtle areas for improvement.
Schedule case review meetings monthly or bi-monthly. More frequent meetings may be necessary in busy practices or during times of high staff turnover. The structure of case reviews can vary based on the practice. Allowing practitioners to present challenging or interesting cases—including patient history, treatment performed, outcomes and any complications—is a great way to encourage dialogue and ownership from the team. During these reviews, it is important to encourage a collaborative discussion where team members can ask questions, offer insights and suggest alternative approaches. Identify key takeaways and best practices from each case; document these to inform future protocols and training. Incorporate patient feedback to inform case reviews and skill assessments. Positive feedback can reinforce good practices, while negative feedback can highlight areas needing attention.
Staff members and employees are vital to your operations, but they also represent a potentially significant risk. When hiring unqualified staff, the business is exposed to the potential of mishandling patient information and safety risks related to treatment. You need to know who you are hiring and thoroughly understand their treatment strengths and areas for improvement. During the hiring process, ensure you perform due diligence. Conduct thorough background checks to ensure employees are qualified and verify clinicians have earned proper credentials and have a history of integrity by contacting prior employees and performing skills checks. During employment, monitor license expiration and hold your team accountable to stay current.
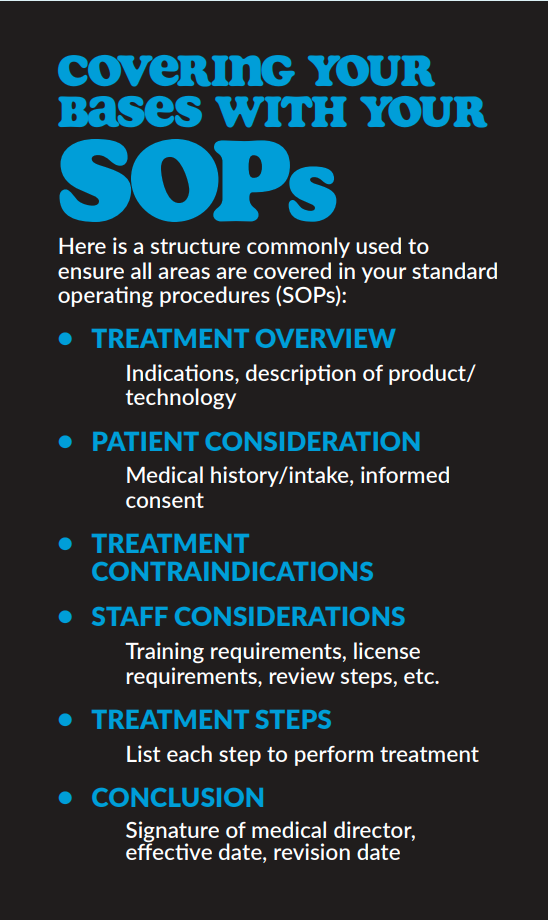
Develop and maintain comprehensive standard operating procedures (SOPs) for every procedure offered at your medical spa. These should cover everything from patient consultation to treatment and post-treatment care. Ensure that all staff are familiar with these procedures and follow them strictly. The practice’s medical director should have final say regarding your medical protocols. Ensure your SOPs have been written according to the medical director’s specifications, as these documents will be the foundation of your team’s training and treatment expectations.
The treatment SOPs should include robust information on patient screening protocols. This includes taking detailed medical histories, understanding patient expectations and assessing their suitability for the desired treatment. Special attention should be given to identifying contraindications and potential allergies. In addition, direction should be documented on how to ensure that patients provide informed consent before undergoing any procedure. This involves explaining the procedure, potential risks, expected outcomes and any alternatives. Consent forms should be detailed and understandable.
Establish a system for reporting adverse events, near misses and any deviations from standard procedures. Ensure that this system is confidential and non-punitive to encourage honest reporting. For each incident, perform a root-cause analysis to identify underlying factors. This might involve reviewing patient records, interviewing involved staff and examining protocols. Develop action plans to address identified issues; this could involve revising protocols, implementing additional training or investing in new equipment.
Conduct regular audits of clinical practices, protocols and patient outcomes. Use audit findings to inform training and quality improvement efforts. Are all your state’s regulations being followed? These lapses should be caught in your audits. Is charting being completed as required? Are medical histories being documented? Maintain detailed records of skill assessments, case reviews, incident reports and quality improvement initiatives; this ensures transparency and accountability, as well as provides the opportunity to showcase that you are running a compliant and safe business, should the need to demonstrate this arise.
Stay updated on local, state and federal regulations governing medical spas. Ensure that your practice complies with all legal requirements, including licensure, certification and reporting obligations. These regulations can often be complex and are frequently updated. Failure to comply with regulations can result in legal action, heavy fines and the potential of business closure. As a business owner and medical director, it is your responsibility to stay informed. Pay attention to local, state and federal regulations for the medical aesthetics industry. Consider a legal partnership with a business attorney who specializes in medical spa regulation. Their knowledge can provide valuable guidance when ensuring compliance and patient safety.
Maintaining patient safety in medical spas is a continuous commitment that requires diligence, education and a proactive approach. By implementing these guidelines, medical spa owners and practitioners can provide a safe and exceptional experience for their patients. Remember, the foundation of a successful practice is built on trust, safety and the well-being of your patients.
Taylor Siemens, NP-C, a board-certified nurse practitioner recognized by the American Association of Nurse Practitioners and clinical advisor for the American Med Spa Association, is a dynamic force in the world of aesthetic medicine. As the vice president of operations at Vitalyc Medspa and the founder of My Aesthetic Training, she seamlessly marries the expertise of a practitioner of medicine with that of a multi-site business operator. Siemens’s journey into aesthetic medicine commenced as an operating room nurse specializing in facial plastic surgery. Through her diverse patient interactions, Taylor has honed a profound understanding of the aging process, fueling her skillset in crafting comprehensive, multi-modality treatment solutions that align seamlessly with patients’ aesthetic objectives.
AmSpa Members receive QP every quarter. Learn how to become a member and access the resources you need to succeed in the medical aesthetics industry.
Related Tags
Medical spa news, blogs and updates sent directly to your inbox.

Clinical
By Belmar Pharma SolutionsYour bustling, successful practice is full of women who really care about their appearance, and they trust ...

Clinical
Win Free Exosomes → Simply Register for the Free Exosome Masterclass By MedResultsIn today’s rapidly evolving aesthetic landscape, one ...

Clinical
With Molly Muecke, RN, MSN, NP-CMicroneedling is a popular aesthetic treatment offered in 79% of med spas (2024 Medical Spa ...

Clinical
On November 5, 2025, Merz Aesthetics announced that Ultherapy PRIME® gained U.S. Food and Drug Administration (FDA) clearance to improve ...