-
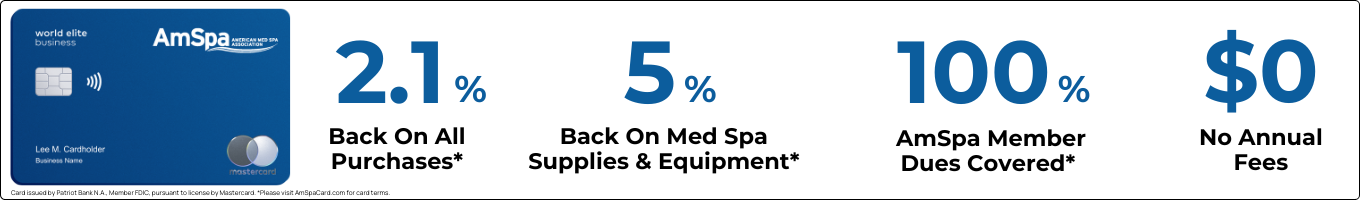
Membership
Become a Member
Show your committment to patient safety, legal compliance and community over competition.
-
Training
Join and Save
AmSpa members receive preferred pricing on all AmSpa live and virtual trainings.
-
Blog & News
Latest Blog Posts
View All PostsDon't Miss an Update
Get the latest news and information about safe, legal practice in medical aesthetics directly in your inbox.
-
Resources
Ready to Get Started?
Get access to med spa laws, in-person and online training and more!
- Contact Us
- Become A Member